The Checklist
If your goal is to free yourself from pain or fatigue...
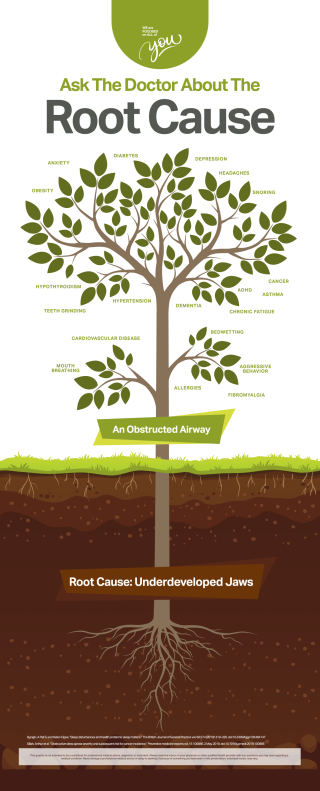
You very likely have an airway problem. Most people do. If you ever had your wisdom teeth removed, that is a sign that you have an underformed jaw. As a consequence, you likely have a shrunken airway that is prone to closing off when you sleep. Why is it so common for people to have underformed jaws? Researchers think that it is because we eat insufficient fiber and roughage as children, and hence do not experience the normal hypertrophy (bulking up) of the jaw bones.
Our airways are further compromised by chronic inflammation due to pollution and an inflammatory western diet.
When our airway is shrunken, it closes off during sleep. This leads to a bad night of sleep. Research tells us that a single bad night of sleep means you are not at your best the next day. It means your immune system is not functioning at 100%. It means you are more prone to cancer and heart disease and Alzheimers.
The tragedy is that when you have an airway problem, you can get a bad night of sleep every night, your entire life! Such people carry huge increases in chronic diseases like obesity, diabetes, cancer, heart disease, infections, autoimmune disease. They also feel lousy. MANY of the people with airway problems suffer from chronic fatigue, headaches, fibromyalgia, jaw pain, allergies, anxiety, depression, and a host of other maladies. They frequently are taking multiple medicines for downstream effects, like sleeping pills, anxiety or depression medicines, or pain pills. Unfortunately, there is no sleeping pill that fixes poor sleep or that makes you function better the next day.
About 90% of people with airway problems are unaware they have a problem.
What are signs that YOU may have an airway problem?
The Signs That You Could Have an Airway Problem
- snoring
- audible breathing (without snoring)
- allergies
- insomnia
- use of sleeping medicines
- night time urination
- dry mouth
- mouth breathing
- nasal congestion
- gum disease
- headache
- fibromyalgia
- pain syndromes
- musculoskeletal pain (knees, hips, more generalized)
- jaw pain
- anxiety
- depression
- obesity
- Atherosclerosis (caused by snoring)
- dementia
- other chronic diseases
Answer this Sleep Health Questionnaire to See if You Might Have a Breathing Problem
- Have you ever been told that you snore or have sleep apnea?
- Does anyone in your family suffer from sleep apnea?
- Do you ever get headaches or have sore teeth or sore jaws?
- Do you take medications/supplements or over the counter sleep aids?
- Is it hard for you to fall asleep? Do you wake up during your sleep? Do you feel unrested when you wake up in the morning?
If your answer to any of these questions is YES, then you may well have a sleep or airway problem.
Doctors are getting better at identifying airway, breathing, and sleep problems but we have a very long way to go. Increasingly, people are getting diagnosed with Obstructive Sleep Apnea (OSA) and getting onto a Continuous Positive Airway Pressure (CPAP) machine. This is a good thing, because CPAP is the gold standard treatment for OSA. It should be the #1 option considered for airway problems. But there are many problems:
Problems with Conventional Medicine and CPAP for Sleep Apnea
- Conventional sleep testing is good but can underdiagnose sleep apnea. If you wake up every 15 minutes every night, you still don't qualify as having official sleep apnea! But you surely will have health consequences and not live your best life, compared to if you did not wake up at all during the night.
- Over 50% of patients fail to wear their CPAP for the flimsy recommended time of at least 20 hours per week (4 hrs per day x 5 days per week). We need 8 hours of sleep, not 4 by the way.
- Getting a CPAP and keeping it maintained can be a logistical nightmare
- CPAP machines are highly regulated with lots of red tape, and they can be super expensive
So what can you do about your own airway, breathing, and sleep? Read on...
Checklist to Identify and Fix Your Airway, Breathing, and Sleep Problems
- 1. Identify if you might have a problem with breathing in your sleep. If you snore, you have a problem. If you have insomnia, you likely have a problem. See our above reverse checklist: The Signs That You Could Have an Airway Problem, and also see the Sleep Health Questionnaire. If you have any of these signs, they there is a good chance you have an airway or breathing problem.
- 2. Test your breathing at night by using the free app SnoreLab. It listens to your sleep and tells how much you may be snoring.
- 3. Tell your doctor or provider about your concerns. Request a sleep study.
- 4. Know your Apnea Hypopnea Index (AHI). This is the score that you get from a sleep study. This is the number of times you pause greater than 10 seconds in your breathing. These pauses lead to significant disruption of sleep. Whether your doctor or provider diagnoses you with Obstructive Sleep Apnea or not, if your AHI is greater than 1, then you have a big opportunity to improve your sleep! If your AHI is 1 or less, then you are done with this checklist!
- 5. Optimize your sleep routine. Follow a lifestyle checklist for better sleep, such as:
Set your bedtime so you can get a full 7-9 hours of sleep
Avoid eating before bed
Wash your nose at nighttime before going to bed using saline sprays such as Xlear
Avoid sleeping pills of all kinds. There is no sleeping pill that improves restfulness, with the exception of melatonin for jet lag.
Get the bedroom right: Keep your bedroom cool, quiet, and free of screens. Close windows to prevent allergens from entering room. Use a white noise or pink noise machine.
Avoid screens and bright or blue light before bed.
Avoid caffeine for 10 hours before bed.
Sleep trackers like Ouararing, Apple watches can help - 6. If you have sleep apnea, go with a CPAP. Ask for newer, more sophisticated versions that automate the amount of pressure based on your comfort. Experiment with different masks. Practice wearing your CPAP machine as much as you can, so that you can get used to it.
- 7. Get your airway evaluated. You need to find a specialist who is an expert in the airway. This can be hard because there is no clear airway specialization. Look for providers who are certified with either AAPMD - American Acedemy of Physiological Medicine and Dentistry, or the AADSM - American Academy of Dental Sleep Medicine. You can use this resource to find doctors who are board certified in Craniofacial Dental Sleep Medicine. You can use this resource to find doctors who are board certified in Craniofacial Dental Sleep Medicine.
- 8. Fix the underlying problems, using therapies recommended by your airway specialist, such as
* custom fitted oral appliance
* myofunctional therapy
* weight loss and anti-inflammation by switching to a whole foods, plant based diet
* breathing exercises
* taping your mouth closed at night - 9. Learn more about the airway. Some good books:
Root Cause by Ryan Robinson
Breath by James Nestor
Oxygen Advantage by Patrick G McKeown
Clinical Protocol: Airway & Sleep
This protocol consists of the questions we can monitor longitudinally, to make this checklist happen, in the clinical setting. These questions can be asked by a patient navigator/care manager, or by a health chatbot.
- weekly: How do you rate your sleep overall? [0-10]
- weekly: We recommend you use the free app SnoreLab. Have you used this yet?
- if no, weekly: On your smart phone, please download the app SnoreLab. It is free to use and works well! If you have trouble, please call your care manager.
- if yes, weekly: What is your typical Snore Score for the week?
- monthly: For optimal sleep, we recommend that you work with your provider to get 8 hours of natural sleep per night, without sleeping pills or other substances. Have you worked with your health care team to get a better night sleep naturally?
- if yes, weekly: What sleep behaviors are you working to improve?
- if sleep behaviors listed, weekly: You are working on these sleep behaviors, correct? [list the behaviors]
- if no: repeat: What sleep behaviors are you working to improve?
- if yes, weekly: How many days in the last week were you able to achieve optimal sleep behaviors?
- monthly: Are you using any sleeping pills or other substances?
- if yes: Which sleeping pills or substances are you using? How frequently do you take your sleeping pills?
- weekly: How many hours of restful, natural sleep are you getting per night?
- monthly: We recommend you get a recent sleep study to measure how many times you awaken per hour of sleep. Have you recently gotten a sleep study?
- if no, monthly: Please contact our office to ask for help setting up a sleep study.
- if yes, monthly: what was your AHI score [Apnea Hypopnea Index]?
- if yes, monthly: what was the lowest oxygen saturation?
- if AHI >= 1 and AHI < 5, monthly: On your recent sleep study, you did not qualify as having sleep apnea, but you did pause in your breathing [AHI] times per hour, which is too much for optimal health. We recommend you get your airway evaluated by an airway specialist, and that you consider pursuing some therapy with your doctor or provider, such as CPAP, an oral appliance, weight loss, or other approach. Do you already have a plan or appointment to make that happen?
- if AHI >= 5, monthly: You have [OSA severity] sleep apnea. We recommend you get your airway evaluated by an airway specialist, and that you consider pursuing some therapy with your doctor or provider, such as CPAP, an oral appliance, weight loss, or other approach. Do you already have a plan or appointment to make that happen?
- monthly: Are you currently using a CPAP?
- monthly: We recommend using CPAP the entire night of sleep. How many hours per night are you using it?
- if using CPAP, weekly: How many nights in the last 7 days did you use your CPAP at least 6 hours?
- monthly: Are you currently using a custom fitted oral appliance?
- monthly: We recommend using CPAP the entire night of sleep. How many hours per night are you using it?
- if using oral appliance, weekly: How many nights in the last 7 days did you use your oral appliance at least 6 hours?
- monthly: Did you see a doctor who specializes in the airway recently?
- if no, Please make an appointment with a doctor who specializes in the airway. If you need assistance making this happen, please contact our office.
- monthly: Are you overweight?
- If yes, monthly: Are you transitioning to a whole foods, plant-based diet rich in fruits, vegetables, intact whole grains, legumes, and nuts and seeds?
- if yes, weekly: In the last 7 days, how many days did you eat mostly whole foods, plant-based diet rich in fruits, vegetables, intact whole grains, legumes, and nuts and seeds?
- If yes, monthly: Are you transitioning to a whole foods, plant-based diet rich in fruits, vegetables, intact whole grains, legumes, and nuts and seeds?
Podcast
Listen to a podcast about this checklist
Root Cause Banner from the Waiting Room of Pain and Sleep Therapy Center
Contributors

Ryan P Robinson, DDS, DABCP, DABDSM, DABCDSM, QOM-D
Ryan Robinson is a specialist in a field that does not exist officially: airway medicine and dentistry. He has a rare triple board certification in dentistry, craniofacial pain and dental sleep medicine. He is the founder of the Pain and Sleep Therapy Center in Wilmington, Delaware. In 2021, he published The Root Cause: Discover The Why Behind Your TMJ And Sleep Problems

David Donohue, MD MS FACP DipABLM @WellDrDave
Dave is the creator of healthrules.org and helped build this checklist. He is a primary care internist, fellow of the American College of Physicians, and a diplomate of the American Board of Lifestyle Medicine. Dave has a masters in molecular biology from Stanford, and he worked 15 years in software architecture. Dave is Chief Medical Officer of Progressive Health of Delaware and a founder of the Lifestyle Medicine Network.
...with the help of our summer intern, Ryaan Bennani!
Handout
This handout can be useful for anyone who might have sleep disordered breathing, to help the whole medical team focus on the steps to improve breathing and fix the underlying health problems.
References
Jones, Jeffrey M. “In US, 40% get less than recommended amount of sleep.” Well Being 19 (2013).
Harmon, Katherine. “Rare genetic mutation lets some people function with less sleep.” Sci Am (2009).
Walker, Matthew. Why we sleep: Unlocking the power of sleep and dreams. Simon and Schuster, 2017.
Leproult, Rachel, and Eve Van Cauter. “Effect of 1 week of sleep restriction on testosterone levels in young healthy men.” Jama 305, no. 21 (2011): 2173-2174.
Kloss, Jacqueline D., Michael L. Perlis, Jessica A. Zamzow, Elizabeth J. Culnan, and Clarisa R. Gracia. “Sleep, sleep disturbance, and fertility in women.” Sleep medicine reviews 22 (2015): 78-87.
Martin, Bruce J. “Effect of sleep deprivation on tolerance of prolonged exercise.” European journal of applied physiology and occupational physiology 47, no. 4 (1981): 345-354.
Milewski, Matthew D., David L. Skaggs, Gregory A. Bishop, J. Lee Pace, David A. Ibrahim, Tishya AL Wren, and Audrius Barzdukas. “Chronic lack of sleep is associated with increased sports injuries in adolescent athletes.” Journal of Pediatric Orthopaedics 34, no. 2 (2014): 129-133.
Van Cauter, Eve, Karine Spiegel, Esra Tasali, and Rachel Leproult. “Metabolic consequences of sleep and sleep loss.” Sleep medicine 9 (2008): S23-S28.
AlDabal, Laila, and Ahmed S. BaHammam. “Metabolic, endocrine, and immune consequences of sleep deprivation.” The open respiratory medicine journal 5 (2011): 31.
Eugene, Andy R., and Jolanta Masiak. “The neuroprotective aspects of sleep.” MEDtube science 3, no. 1 (2015): 35.
Alhola, Paula, and Päivi Polo-Kantola. “Sleep deprivation: Impact on cognitive performance.” Neuropsychiatric disease and treatment (2007).
Goel, Namni, Hengyi Rao, Jeffrey S. Durmer, and David F. Dinges. “Neurocognitive consequences of sleep deprivation.” In Seminars in neurology, vol. 29, no. 04, pp. 320-339. © Thieme Medical Publishers, 2009.
Williamson, Ann M., and Anne-Marie Feyer. “Moderate sleep deprivation produces impairments in cognitive and motor performance equivalent to legally prescribed levels of alcohol intoxication.” Occupational and environmental medicine 57, no. 10 (2000): 649-655.
Tefft, Brian C. “Acute sleep deprivation and culpable motor vehicle crash involvement.” Sleep 41, no. 10 (2018): zsy144.
Goel, Namni, Hengyi Rao, Jeffrey S. Durmer, and David F. Dinges. “Neurocognitive consequences of sleep deprivation.” In Seminars in neurology, vol. 29, no. 04, pp. 320-339. © Thieme Medical Publishers, 2009.
Yoo, Seung-Schik, Ninad Gujar, Peter Hu, Ferenc A. Jolesz, and Matthew P. Walker. “The human emotional brain without sleep—a prefrontal amygdala disconnect.” Current Biology 17, no. 20 (2007): R877-R878.
Gordon, Amie M., and Serena Chen. “The role of sleep in interpersonal conflict: do sleepless nights mean worse fights?.” Social Psychological and Personality Science 5, no. 2 (2014): 168-175.
Give Feedback
Is this checklist missing something? Do you have a success story from trying this checklist out? We would like to hear your feedback.