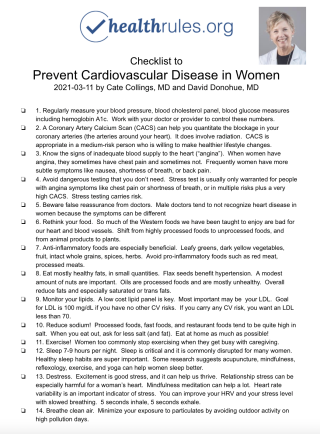
The Checklist
If your goal is to avoid the leading killer of women...
Cardiovascular disease or CVD refers to diseases of the blood vessels to the heart (heart attack, CHF), brain (stroke, TIA), or other organs (peripheral artery disease, aortic aneurysms). CVD is usually due to accumulation of cholesterol plaque and inflammation. The most common cause of death from CVD is from heart disease, and we sometimes use the terms heart disease and CVD interchangeably.
CVD claims the lives of 1 in 3 women in the United States and globally. That is more deaths than from all forms of cancer combined.
CVD doesn’t happen all of a sudden. It starts young in life, with fatty streaks depositing in children who eat Western style foods. It is usually without symptoms until later in life. But when kids develop obesity, elevated lipids, or diabetes, it is a sign that heart disease is in process.
Sometimes CVD first shows itself during pregnancy, when early CVD can manifest with preterm birth, miscarriage, or still birth. Some conditions during or shortly after pregnancy are harbingers for greater risk of future CVD: gestational diabetes, hypertension, preeclampsia. Pregnancy can be thought of as an early stress test of your heart, and any of these signs can signify likely early CVD.
What causes CVD? The main causes of CVD in women and men are high blood lipids and cholesterol, high blood pressure, diabetes and high blood glucose, obesity, inflammation, and toxins like tobacco. Your genes play a role and if you have a lot of CVD in your close relatives, you may have extra risk yourself.
Most people are not aware that you can change your genetics! Health lifestyle behaviors can literally turn on healthier genes and turn off unhealthy genes.
Fortunately, CVD can be prevented and even reversed at almost any stage of a girl's or woman's life. How can I do that you ask?
Checklist to Prevent Cardiovascular Disease in Women
- 1. Regularly measure your key heart metrics to make sure you are keeping them well controlled, especially blood pressure, blood cholesterol panel, blood glucose measures including hemoglobin A1c. Work with your doctor or provider to control these numbers.
- 2. A Coronary Artery Calcium Scan (CACS) can help you quantitate the blockage in your coronary arteries (the arteries around your heart). It does involve radiation. CACS is appropriate in a medium-risk person who is willing to make healthier lifestyle changes. CACS can help us decide how urgent it might be to intervene with medications or big lifestyle changes.
- 3. Know the signs of inadequate blood supply to the heart (“angina”). When women have angina, they sometimes do not develop the classic symptom of chest pain. Frequently women have more subtle symptoms like nausea, shortness of breath, or back pain.
More so than men, women can frequently have small vessel disease which does not show up on stress imaging or coronary catheterization. - 4. Avoid dangerous testing that you don’t need. Stress test is usually only warranted for people with angina symptoms like chest pain or shortness of breath, or in multiple risks plus a very high CACS. Stress testing carries risk. False positives can lead to harm from unnecessary procedures and worry.
- 5. Beware false reassurance from doctors. Male doctors tend to not recognize heart disease in women because the symptoms can be different, and because women can frequently have small vessel disease which does not show up as easily on stress imaging or coronary catheterization.
- 6. Rethink your food. So much of the Western foods we have been taught to enjoy are bad for our heart and blood vessels. Shift from highly processed foods to unprocessed foods, and from animal products to plants. Research suggests you can almost totally neutralize your chances of a heart attack if you make big enough changes to your diet alone.
- 7. Anti-inflammatory foods are especially beneficial. Leafy greens, dark yellow vegetables, fruit, intact whole grains, spices, herbs. Avoid pro-inflammatory foods such as red meat, processed meats.
- 8. Eat mostly healthy fats, in small quantities. Flax seeds benefit hypertension. A modest amount of nuts are important. Oils are processed foods and are mostly unhealthy. Extra Virgin Olive Oil is the one to cook with, but again small quantities. Overall reduce fats and especially saturated or trans fats.
- 9. Monitor your lipids. A low cost lipid panel is key. Most important is probably your LDL. Goal for LDL is 100 mg/dL if you have no other CV risks. If you carry any CV risk, you want an LDL less than 70.
- 10. Reduce sodium! Processed foods, fast foods, and restaurant foods tend to be quite high in salt. When you eat out, ask for less salt (and fat). Eat at home as much as possible!
- 11. Exercise! Women too commonly stop exercising when they get busy with caregiving. Try to avoid sacrificing your own exercise in favor of getting everyone else to exercise.
- 12. Sleep 7-9 hours per night. Sleep is critical and it is commonly disrupted for many women. Healthy sleep habits are super important. Some research suggests acupuncture, mindfulness, reflexology, exercise, and yoga can help women sleep better. Sleeping pills are generally not thought to be restorative or healthy.
- 13. Destress. Excitement is good stress, and it can help us thrive. Relationship stress can be especially harmful for a woman’s heart. Mindfulness meditation can help a lot. Heart rate variability is an important indicator of stress. You can improve your HRV and your stress level with slowed breathing. 5 seconds inhale, 5 seconds exhale.
- 14. Breathe clean air. Minimize your exposure to particulates by avoiding outdoor activity on high pollution days. When you are able, move away from highways and fossil fueled power plants. Swap out your gas stove. Particulates in the air are a top 10 cause of death, especially death from CVD.
Podcast
Listen to a podcast about this checklist
Contributors
This checklist was created by:

Cate Collings, MD
Dr. Catherine Collings is a cardiologist and and president of the American College of Lifestyle Medicine. She is Director of Lifestyle Medicine at El Camino Health Medical Network and leads the Lifestyle Medicine primary care practice.

David Donohue, MD MS FACP DipABLM
Dave is the creator of healthrules.org and helped build this checklist. He is a primary care internist, fellow of the American College of Physicians, and a diplomate of the American Board of Lifestyle Medicine.
Handout
References
Kyker KA, Limacher MC. Gender differences in the presentation and symptoms of coronary artery disease. Curr Womens Health Rep. 2002 Apr;2(2):115-9. PMID: 12116600.
World Health Federation. CVD Facts Tips. https://www.world-heart-federation.org/resources/women-cvd-facts-tips/. Accessed 202-03-18
Nowakowski S1, Meers J1, Heimbach E2. Sleep and Women's Health. Sleep Med Res. 2013;4(1):1-22.
Li J, Lee DH, Hu J, Tabung FK, Li Y, Bhupathiraju SN, Rimm EB, Rexrode KM, Manson JE, Willett WC, Giovannucci EL, Hu FB. Dietary Inflammatory Potential and Risk of Cardiovascular Disease Among Men and Women in the U.S. J Am Coll Cardiol. 2020 Nov 10;76(19):2181-2193. doi: 10.1016/j.jacc.2020.09.535. PMID: 33153576; PMCID: PMC7745775.
Rosengren A, Hawken S, Ounpuu S, Sliwa K, Zubaid M, Almahmeed WA, Blackett KN, Sitthi-amorn C, Sato H, Yusuf S; INTERHEART investigators. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet. 2004 Sep 11-17;364(9438):953-62. doi: 10.1016/S0140-6736(04)17019-0. PMID: 15364186.
Hayes RB, Lim C, Zhang Y, Cromar K, Shao Y, Reynolds HR, Silverman DT, Jones RR, Park Y, Jerrett M, Ahn J, Thurston GD. PM2.5 air pollution and cause-specific cardiovascular disease mortality. Int J Epidemiol. 2020 Feb 1;49(1):25-35. doi: 10.1093/ije/dyz114. PMID: 31289812; PMCID: PMC7124502.
Give Feedback
Is this checklist missing something? Do you have a success story from trying this checklist out? We would like to hear your feedback.